You buy the cleanser everyone raves about. You apply the spot treatment religiously. Yet, every month, like clockwork, a painful, deep bump appears in the exact same spot on your chin.
It is exhausting. Treating acne feels like a losing battle when you are using the wrong weapons. If you are treating a hormonal issue with surface-level antibacterial creams, you aren’t just wasting money—you’re likely damaging your skin barrier in the process.
The key to clear skin isn’t “more products.” It is correct diagnosis. This guide breaks down the biological differences between hormonal acne vs. bacterial acne so you can finally choose the treatment path that actually works.
The Core Difference: Is It Internal or External?
At a high level, the difference lies in the root cause. Bacterial acne is largely an external issue involving clogged pores and hygiene. Hormonal acne is an internal issue involving chemical messengers (androgens) that stimulate oil glands from the inside out.
While they look similar to the untrained eye, their behavior is distinct.
Here is the quick breakdown:
| Feature | Hormonal Acne | Bacterial Acne |
| Primary Location | Lower face: Jawline, Chin, Neck (U-Zone) | Upper face: Forehead, Nose, Cheeks (T-Zone) |
| Appearance | Deep, painful cysts or nodules; often no “head” | Surface whiteheads, blackheads, or small pustules |
| Timing | Cyclical; flares up monthly (pre-period or ovulation) | Random; consistent presence or flares after sweating |
| Root Cause | Internal androgen spikes, cortisol (stress) | Clogged pores, excess sebum, C. acnes bacteria |
| Response to Topicals | Stubborn; creams often don’t reach the source | Responsive; improves with exfoliation and hygiene |
What is Bacterial Acne? (The “Surface” Problem)
Bacterial acne happens when your pores get blocked by dead skin cells and excess oil (sebum). This blockage creates an oxygen-free environment perfect for Cutibacterium acnes (formerly P. acnes) to thrive.
The bacteria multiply, causing inflammation and pus. This results in the classic whitehead or red bump. It is often triggered by external factors:
-
Touching your face.
-
Dirty pillowcases or phone screens.
-
Heavy makeup or comedogenic (pore-clogging) moisturizers.
What is Hormonal Acne? (The “Deep” Problem)
Hormonal acne is driven by fluctuations in your body’s chemistry. Specifically, spikes in androgens (like testosterone) trigger your sebaceous glands to produce thicker, stickier oil.
Because this happens deep within the pore, the resulting breakout is often deep within the skin. These are the painful, throbbing cysts that never seem to come to a head. Common triggers include:
-
Menstrual cycle fluctuations.
-
Polycystic Ovary Syndrome (PCOS).
-
High stress (Cortisol spikes).
-
Dietary triggers like dairy or high-glycemic sugar.
Location Matters: Acne Face Mapping 101
Your skin offers clues through “Face Mapping.” Where you break out is often just as important as how you break out.
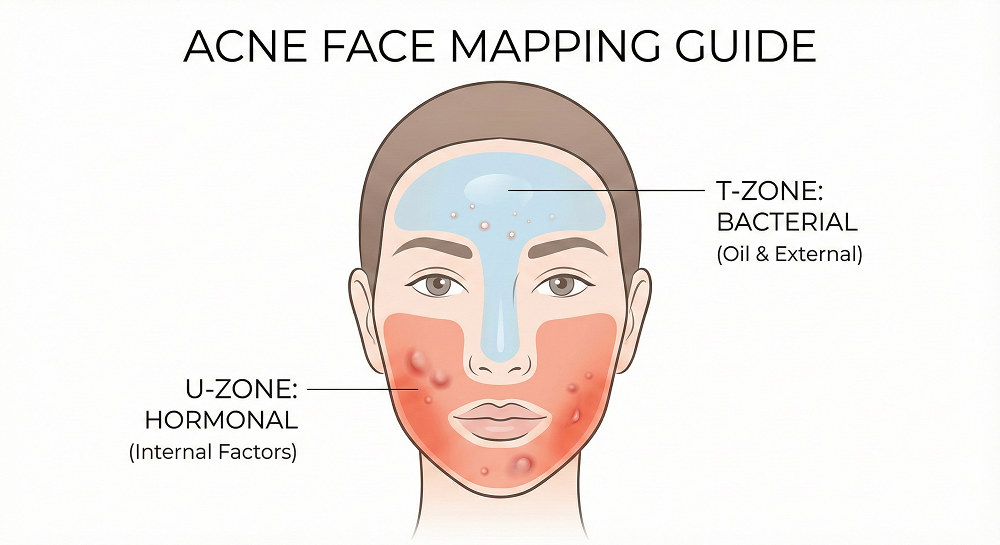
The T-Zone (Forehead & Nose)
Breakouts here are typically bacterial or fungal. The forehead has a high density of oil glands but is also prone to sweat and friction from hats or hair products (pomade acne). If you see whiteheads here, look at your hygiene habits first.
The U-Zone (Cheeks, Jawline & Chin)
This is the classic “beard area.” Breakouts along the jawline and chin are the hallmark of hormonal activity. The oil glands here are hypersensitive to androgen spikes. If you are strictly breaking out here, no amount of face washing will fix the internal surge of hormones.
Diagnostic Checklist: 5 Signs to Watch
Still unsure? Use this checklist to narrow it down. You likely have Hormonal Acne if:
-
The timing is predictable: You can almost mark your calendar for when a breakout will appear (usually a week before your cycle).
-
It hurts: The pimples are tender to the touch and feel like deep lumps under the skin.
-
Standard treatments fail: You have tried Benzoyl Peroxide or antibiotics, but the acne returns immediately after you stop.
-
You are stressed: You notice flare-ups during high-stress periods (exams, work deadlines), which points to Cortisol.
-
It’s mostly on the lower face: Your forehead is relatively clear, but your chin is congested.
Treatment Protocols: Treating the Root Cause
Once you know the enemy, you can choose the right weapon. Here is how to approach each type effectively.
How to Treat Bacterial Acne
The goal here is to keep pores clear and kill bacteria.
-
Salicylic Acid (BHA): Dissolves oil inside the pore to prevent clogs.
-
Benzoyl Peroxide: Introduces oxygen into the pore, which kills C. acnes bacteria.
-
Blue Light Therapy: Kills surface bacteria without irritation.
-
Hygiene Habits: Change your pillowcase every 2-3 days and clean your makeup brushes.
How to Treat Hormonal Acne
Topical treatments struggle here because the problem is internal.
-
Retinoids (Adapalene/Tretinoin): Speed up cell turnover to prevent the sticky oil from trapping bacteria deep down.
-
Spironolactone: A prescription medication that blocks androgen receptors, stopping the hormonal signal to the oil glands.
-
Dietary Changes: Reducing dairy and sugar can lower insulin spikes, which often trigger acne hormones.
-
Stress Management: Lowering cortisol levels is a legitimate skincare strategy.
Note: For more insights on building a routine that supports skin health, check out our resources at Meo Beauty.
The “Double Whammy”: Can You Have Both?
Yes, absolutely. In fact, they often feed each other.
Hormonal fluctuations increase oil production. That excess oil then gets trapped by dead skin cells, creating a feast for bacteria. The result? A mixture of deep cysts (hormonal) and surface whiteheads (bacterial).
If you have both, start by repairing your moisture barrier. Aggressively attacking your skin with too many acids will only increase inflammation, making both types of acne worse.
When to See a Professional
Home care has limits. You should see a dermatologist if:
-
You have deep, painful nodules (these can cause permanent scarring).
-
Your acne is affecting your mental health or self-esteem.
-
Over-the-counter (OTC) treatments haven’t worked after 3 months of consistent use.
Professionals can offer stronger tools like prescription Retinoids, Spironolactone, or Accutane (Isotretinoin) to break the cycle.
Frequently Asked Questions (FAQ)
How do I tell if my acne is hormonal or bacterial?
Look at the location and timing of the breakout.
Hormonal acne typically appears on the lower face (jawline/chin) as deep cysts and flares up monthly. Bacterial acne appears anywhere (often T-zone) as surface whiteheads and is consistent rather than cyclical.
Does salicylic acid work on hormonal acne?
It is generally less effective for hormonal cysts.
Salicylic acid treats the surface pore, but hormonal acne forms deep internally. While it helps manage surface oil, internal regulators (like Spironolactone) or strong retinoids are usually required to stop hormonal breakouts at the source.
Can bacterial acne turn into hormonal acne?
No, but they often overlap.
Bacteria cannot “become” hormones. However, hormonal changes cause excess oil, which feeds bacteria. This creates a cycle where internal imbalances trigger external bacterial infections.
What kills bacterial acne naturally?
Tea Tree Oil and Green Tea Extract.
Tea Tree Oil has proven antimicrobial properties against C. acnes. Green tea (applied topically) reduces sebum production. Honey (specifically Manuka) is also a natural antibacterial agent that soothes inflammation.
For more beauty tips, product reviews, and skincare guides, visit us at Meo Beauty.
![Hormonal Acne vs Bacterial Acne Hormonal Acne vs. Bacterial Acne: Identifying Your Root Cause for Clearer SkinYou’ve tried every face wash, spot treatment, and viral skincare hack, but the breakout keeps coming back in the exact same spot. It’s exhausting. It feels like your skin is fighting against you, no matter how clean your routine is.The problem likely isn't your product—it’s your diagnosis.Most people treat all acne the same, blasting their skin with drying agents that only work on surface bacteria. But if your breakout is driven by internal chemistry, no amount of face wash will fix it. To clear your skin, you must first distinguish between Hormonal Acne (internal) and Bacterial Acne (external).This guide breaks down the differences, maps your symptoms, and helps you match the cure to the cause.The Core Differences: Hormonal vs. Bacterial Acne at a GlanceBefore we analyze your specific symptoms, look at the big picture. Hormonal acne is systemic; it’s a body-wide signal. Bacterial acne is often localized and environmental.Here is the quickest way to tell them apart:FeatureHormonal AcneBacterial AcnePrimary LocationLower face, Jawline, Chin, NeckT-Zone, Forehead, Nose, CheeksAppearanceDeep, painful cysts; red nodules; no "head"Whiteheads, blackheads, small red bumpsPrimary TriggerInternal: Androgen spikes, Stress, MenstruationExternal: Clogged pores, Sweat, Dirt, BacteriaBest TreatmentInternal regulators (Spironolactone, Diet)Topical antibacterials (Benzoyl Peroxide, Acids)Note: While these are distinct types, they often overlap. Hormones can increase oil production, which then feeds bacteria. We call this the "Cycle of Convergence," which we will discuss later.[Insert Image: Infographic A - Venn Diagram comparing Internal vs. External triggers]The Face Map: Decoding Your Breakout LocationYour skin is a map. The location of your breakout is often the strongest indicator of its root cause.[Insert Image: Split Screen Face - Left side showing deep jawline cysts, Right side showing forehead whiteheads]The "Beard of Acne" (Jawline & Chin)If your breakouts are concentrated along the jawline, chin, and upper neck—forming a "beard" pattern—this is the classic signature of hormonal acne.The lower face has a high concentration of androgen receptors. When your hormones fluctuate (due to menstruation, stress, or conditions like PCOS), these receptors trigger your oil glands to go into overdrive. This produces deep, inflamed cysts that feel like hard knots under the skin.The T-Zone (The Bacterial Belt)Breakouts on the forehead and nose are typically bacterial or fungal. This area, known as the T-Zone, naturally produces more sweat and oil.However, the cause here is usually external blocking. Think about what touches your forehead:Sweat from workouts.Hair products (conditioners or styling creams).Hats or headbands.When Cutibacterium acnes (the bacteria responsible for acne) gets trapped with sweat and dead skin cells in these pores, you get whiteheads and blackheads.Why am I breaking out on only one side?If you have acne strictly on the left or right cheek, it is almost certainly Acne Mechanica (mechanical friction), which falls under the bacterial umbrella.Common culprits include:Dirty pillowcases: If you sleep on your side, your face presses against fabric accumulating oils and bacteria for 8 hours a night.Smartphones: Holding a phone against your cheek transfers screen bacteria directly to your pores.Hand resting: Leaning your chin or cheek on your hand while working.Symptom Checker: Deep Cysts vs. Surface WhiteheadsLocation matters, but the type of pimple tells the rest of the story.[Insert Image: Interactive Element - "The Acne Decoder Quiz" widget placeholder]The Timing TestHormonal: Is it cyclical? If you notice a flare-up 7–10 days before your period (the Luteal phase), it’s hormonal. This is when progesterone rises and testosterone becomes relatively dominant, spiking sebum production.Bacterial: Is it random? Bacterial breakouts happen whenever a pore gets clogged. If you slept in your makeup or wore a sweaty hat yesterday, and wake up with a pimple today, that is bacterial.The "Squeeze Test" (And Why You Shouldn't Do It)We know you want to pop it. But pause and observe.Hormonal cysts have no "head." They are deep inflammation. If you try to squeeze them, nothing comes out, but they swell and become more painful. You are pushing the infection deeper into the dermis, which causes scarring.Bacterial pimples (pustules) usually have a white or yellow center on the surface. They are superficial infections of the follicle.The "Cycle of Convergence": Can You Have Both?Yes. In fact, most chronic acne sufferers deal with a mix.While we separate them for diagnosis, hormonal fluctuations feed bacterial acne.Here is the biological chain reaction:Hormones: Androgens spike (due to stress or cycle).Oil: Your sebaceous glands produce excess, sticky sebum.Bacteria: C. acnes bacteria, which lives on everyone's skin, feeds on this sebum.Inflammation: The bacteria multiply rapidly, causing the pore to become inflamed and blocked.If you only treat the bacteria (Benzoyl Peroxide), you aren't stopping the oil source. If you only treat the hormones, you might still have existing bacterial overgrowth.Treatment Protocols: Matching the Cure to the CauseOnce you know the source, you can choose the right weapon.[Insert Image: Infographic B - Decision Tree "If acne is X, use Ingredient Y"]Treating Hormonal Acne (Internal Strategy)Topical creams often fail here because the problem is in your bloodstream, not just your pores.Oral Regulators: Dermatologists often prescribe Spironolactone (blocks androgen receptors) or specific birth control pills.Dietary Shifts: Insulin spikes trigger similar hormonal responses. reducing high-glycemic foods (sugar, white bread) and dairy can lower inflammation.Stress Management: Cortisol (the stress hormone) acts like an androgen. Lowering stress is literally skincare.Treating Bacterial Acne (External Strategy)Your goal is to keep the pore clean and the environment hostile to bacteria.Benzoyl Peroxide: The gold standard. It introduces oxygen into the pore, which kills anaerobic bacteria.Salicylic Acid (BHA): Dissolves the "glue" holding dead skin cells together, preventing the clog in the first place.Hygiene: Change pillowcases weekly, wipe down your phone, and wash your face immediately after sweating.Frequently Asked QuestionsWhat is the main difference between hormonal and bacterial acne?Hormonal acne appears as deep cysts on the jawline, while bacterial acne is surface-level whiteheads in the T-zone.Hormonal breakouts are driven by internal androgen spikes, whereas bacterial acne is caused by external factors like sweat, dirt, and clogged pores trapping bacteria.How do I know if my acne is hormonal or fungal?Fungal acne itches intensely and appears as uniform clusters of small red bumps.Unlike hormonal cysts (large/painful) or bacterial zits (varied sizes), fungal acne is actually an infection of the hair follicle by yeast (Malassezia). If standard acne treatments make it worse, it’s likely fungal.Can bacterial acne turn into hormonal acne?No, but hormonal changes can worsen bacterial acne.They have different root causes. However, hormonal spikes increase oil production. Since bacteria eat oil, hormonal issues create the perfect breeding ground for bacterial acne to thrive.What is the best treatment for hormonal acne?Treatments that regulate internal hormone production are most effective.Topical creams struggle to penetrate deep cysts. Options include Spironolactone, oral contraceptives, and dietary changes (low sugar/dairy) to control insulin and androgen levels.Why am I getting acne only on one side of my face?This is likely "Acne Mechanica" caused by physical contact.Common triggers include sleeping on a dirty pillowcase, pressing a smartphone against your cheek, or frequently resting your chin in your hand.](https://meobeauty.net/wp-content/uploads/2025/12/Hormonal-Acne-vs.-Bacterial-Acne-How-to-Tell-the-Difference.png)


